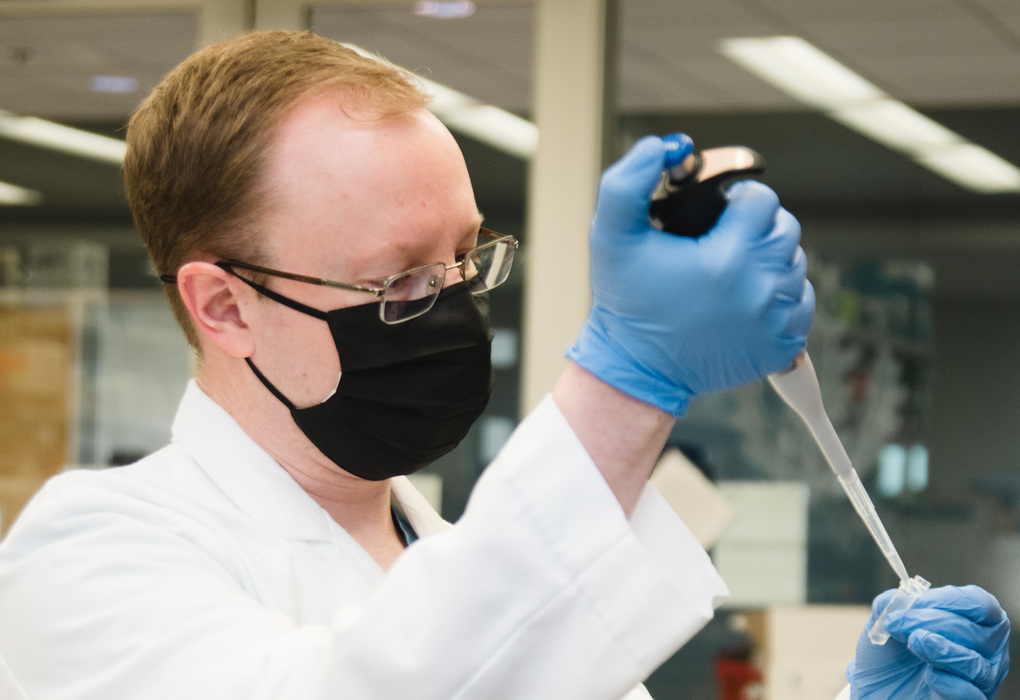
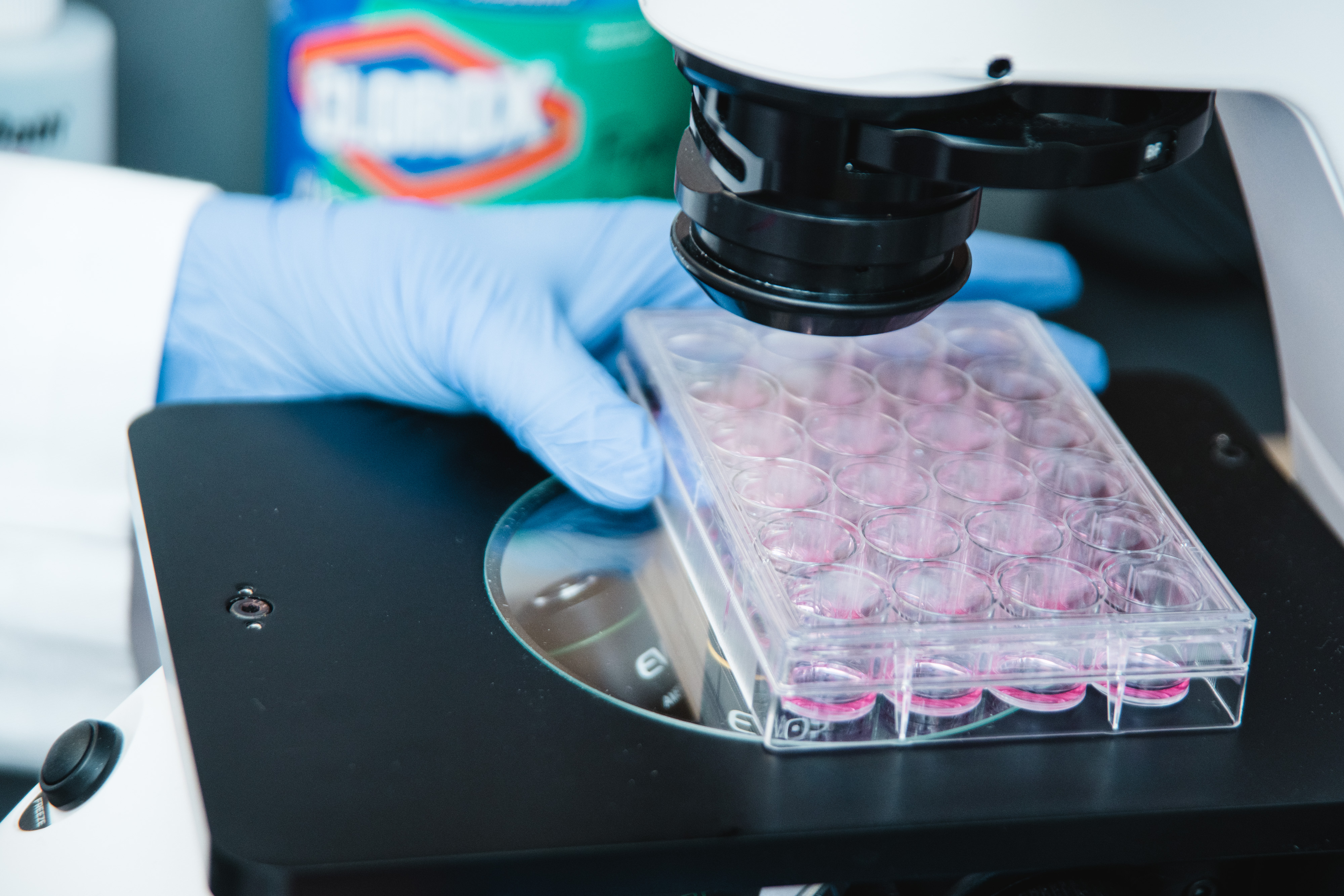
Connecticut Children’s Division of Neurosurgery seeks to better understand disorders that affect the pediatric nervous system. As part of the state’s only health system 100% dedicated to children, we are committed to advancing the field of pediatric neurosurgery. We work with other researchers regionally and nationally to improve pediatric neurosurgical understanding and clinical care.
Core Research Areas
| Brain Tumors |
|
| Patient Outcomes |
|
| Skull, Neck & Spine |
|
Recent Research Breakthroughs
- We identified a unique set of small molecules in the blood stream of pediatric patients with the most common type of brain tumor, juvenile pilocytic astrocytoma. These molecules may be able to screen children for this type of brain tumor without relying on sedated imaging.
- Our group has created a machine learning model capable of screening more than 95% of congenital cranial deformities using only a set of digital photos. This inexpensive and non-invasive screening tool may help reduce the use of CT scans, which expose babies with cranial deformities to potentially harmful radiation.
- We led efforts to define best practices for the healthcare transition process in pediatric neurosurgery.
- We developed and/or validated standardized measurement techniques for children with loose ligaments of the upper neck in Down syndrome and for children with a condition of the junction of the brain and spinal cord known as Chiari malformation.
- We worked with other members of the Pediatric Craniocervical Society to look at growth of the spine after placement of screws and rods to stabilize the spine.
- We worked with other members of the Pediatric Craniocervical Society to develop standards for the use of traction to treat spine deformity as well as how best to manage spinal cord injury in children.
- Healthcare transition is the process of moving from a pediatric to an adult model of health care with or without transfer to a new physician. Dr. Martin led efforts by the American Society of Pediatric Neurosurgeons to evaluate the current practice of healthcare transition among members and to define best practice for transition for pediatric neurosurgical patients.
- Dr. Martin maintains an active interest in disorders involving the craniocervical junction. As a member of the Pediatric Craniocervical Society, Dr. Martin has worked to further our understanding of issues to include:
- Growth of the cervical spine after the placement of spinal instrumentation in children
- The development of measurement standards for complex Chiari malformation and Down syndrome
- Standards for the use of cervical traction in complex spinal stabilization and reconstruction



Sample of Recent Research Publications
- Image processing and machine learning for telehealth craniosynostosis screening…
- Peripheral circulation miRNA expression of pediatric brain tumors and its relat…
- Circulating serum oncologic miRNA in pediatric juvenile pilocytic astrocytoma p…
- In vitro 3D regeneration-like growth of human patient brain tissue
- Safety and efficacy of brainstem biopsy in children and young adults
- Evaluation and treatment of children with radiation-induced cerebral vasculopat…
- Converting Pediatric Patients and Young Adults From a Shunt to a Third Ventricu…
- Predictors of an Extended Length of Stay following an Elective Craniotomy in Ch…
- Growth and alignment of the pediatric subaxial cervical spine following rigid i…
- Standardized method for the measurement of Grabb’s line and clival-canal angle
- Health care transition in pediatric neurosurgery: a consensus statement from th…
- Assessment of craniocervical motion in Down syndrome: a pilot study of two meas…