Agenesis of the corpus callosum occurs when the corpus callosum doesn’t develop or only partially develops. The corpus callosum is a central structure within the brain that serves as a bridge of connecting nerves between the two halves of the brain. It facilitates communication of motor, sensory and cognitive information between the two hemispheres. The corpus callosum begins to form at about 6 weeks of gestation and continues to form from anterior to posterior until approximately 20 weeks of gestation. While the basic structure of the corpus callosum is formed by that time frame, the region continues to develop and thicken into infancy. The development and growth of this region, like other regions within the brain, involves migration and proliferation of different cell types in order for the corpus callosum to form correctly. Agenesis of the corpus callosum (ACC) is one of the most frequent malformations in the brain with a reported incidence ranging between 0.5-70 in 10,000 live births.
Prenatally, ultrasound can have limitations for evaluating the fetal brain due to the overall uniform nature of the brain tissue. As a result, techniques have been created to evaluate the formation of the brain via indirect methods. Firstly, this region is assessed by ultrasound in the mid-trimester during the standard anatomy ultrasound by evaluating the cavum septum pallucidum (CSP). The CSP is a potential fluid filled space within the fetal brain that is located behind and beneath the corpus callosum, above the midbrain and between two leaflets that fuse together in the midline later in development. When the CSP is visualized during prenatal anatomy ultrasound, it reassures that the structures surrounding this space are forming appropriately. Another method for evaluating the presence of the corpus callosum with ultrasound is assessing the pericallosal artery that runs along the superior side of the corpus callosum. As with the CSP, if the corpus callosum is developing normally, the pericallosal artery should have a typical shape and blood flow pattern.
In the setting where a CSP cannot be visualized during a second trimester anatomy ultrasound or the pericallosal artery appears abnormal, the shape of the lateral ventricles can also be helpful to determine the likelihood of an underlying malformation. When the lateral ventricles are teardrop shaped (colpocephaly) or dilated, there is an increased suspicion of an underlying malformation within the brain. Additionally, the third ventricle of the brain is often dilated and superiorly displaced in the setting of ACC. When one or more of these ultrasound findings is abnormal, one of the possible diagnoses is the absence or partial formation of the corpus callosum.
Figure 1. Normal Ultrasound Views
A. Axial view of the fetal brain with normal appearing CSP and normal decompressed 3rd ventricle.
B. Coronal view of the corpus callosum bridging the 2 hemispheres and superior to the CSP
C. Sagittal view of the pericallosal artery coursing above and in close proximity to the intact corpus callosum.
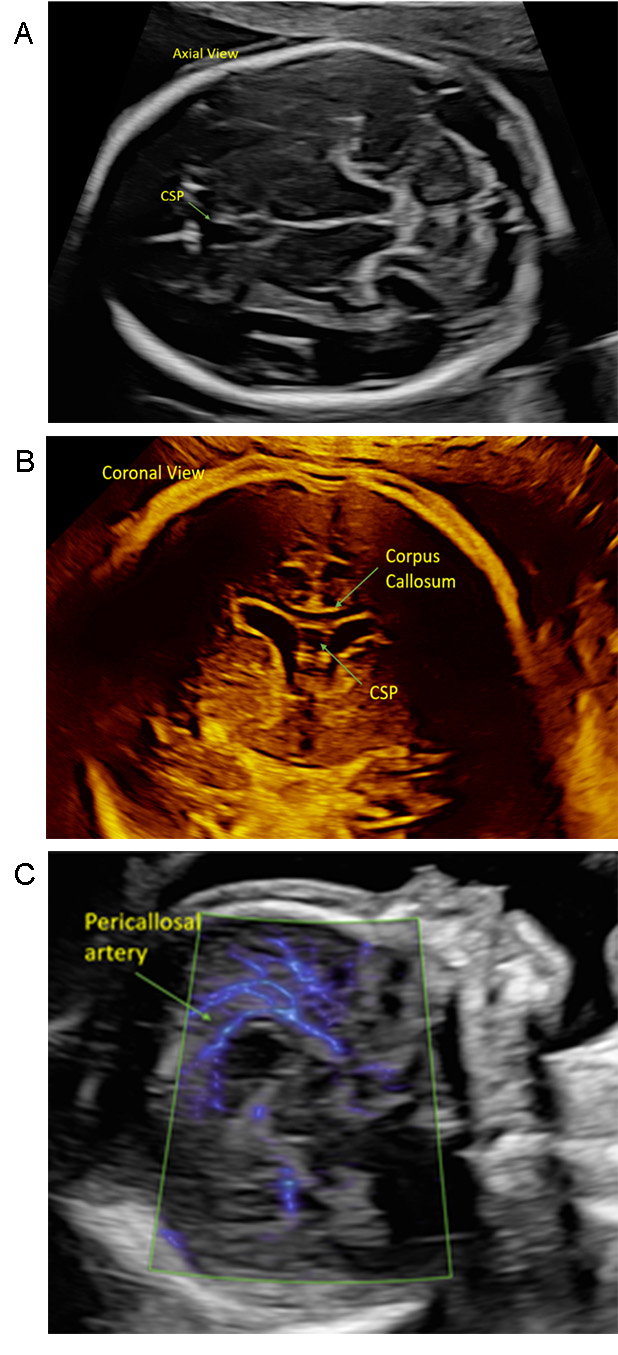
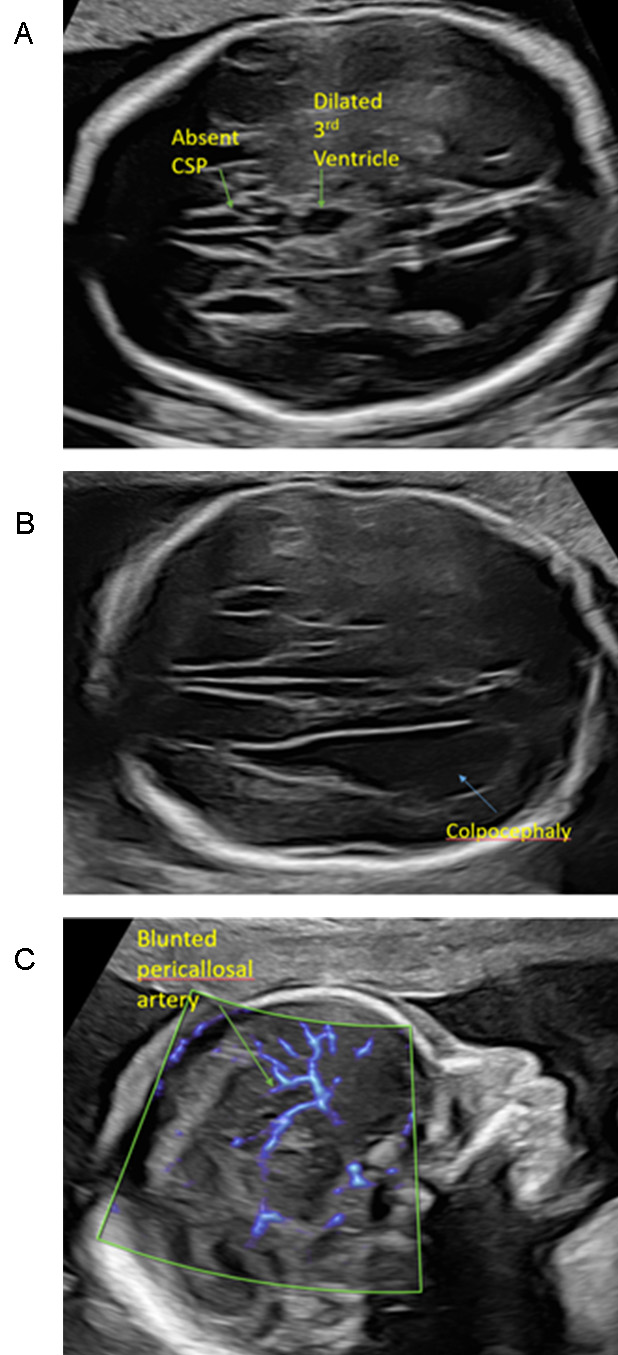
Figure 2. Abnormal Ultrasound Views
A. Region of the CSP without a clear CSP noted. CSP should be an echolucent box, the dilated 3rd ventricle is shown and can be confused for an intact CSP.
B. The posterior horns of the lateral ventricles are disproportionally larger than the anterior horns, creating a “teardrop” appearance termed colpocephaly.
C. Pericallosal artery is blunted in appearance and does not continue posteriorly, instead with differing trajectory superiorly and in a more anterior direction.
MRI is commonly utilized to further evaluate the fetal brain following a suspicious finding on prenatal ultrasound. Imaging of the brain with MRI can be viewed as complementary to ultrasound for evaluation of the nuances for brain development. With MRI, evaluation of the structures of the brain is direct and looks at the structures in question as opposed to ultrasound where indirect ultrasound findings are used. As a result, the presence and integrity of the corpus callosum can be directly visualized. In some cases, the corpus callosum is completely absent and is referred to as agenesis of the corpus callosum (ACC). However, there are other cases where there is one or more portions of the corpus callosum that haven’t formed appropriately referred to as partial agenesis of the corpus callosum (PACC). In addition to evaluation of the corpus callosum, MRI allows for further evaluation of the other structures within the brain for other areas that may have not formed appropriately with higher sensitivity than with ultrasound alone.
Figure 3. Normal MRI for the Corpus Callosum and CSP
A. Coronal image displaying the corpus callosum connecting the 2 brain hemispheres, superior to the CSP
B. Axial view of the CSP and the anterior portion of the corpus callosum
C. Sagittal view of the corpus callosum, with fully developed segments seen
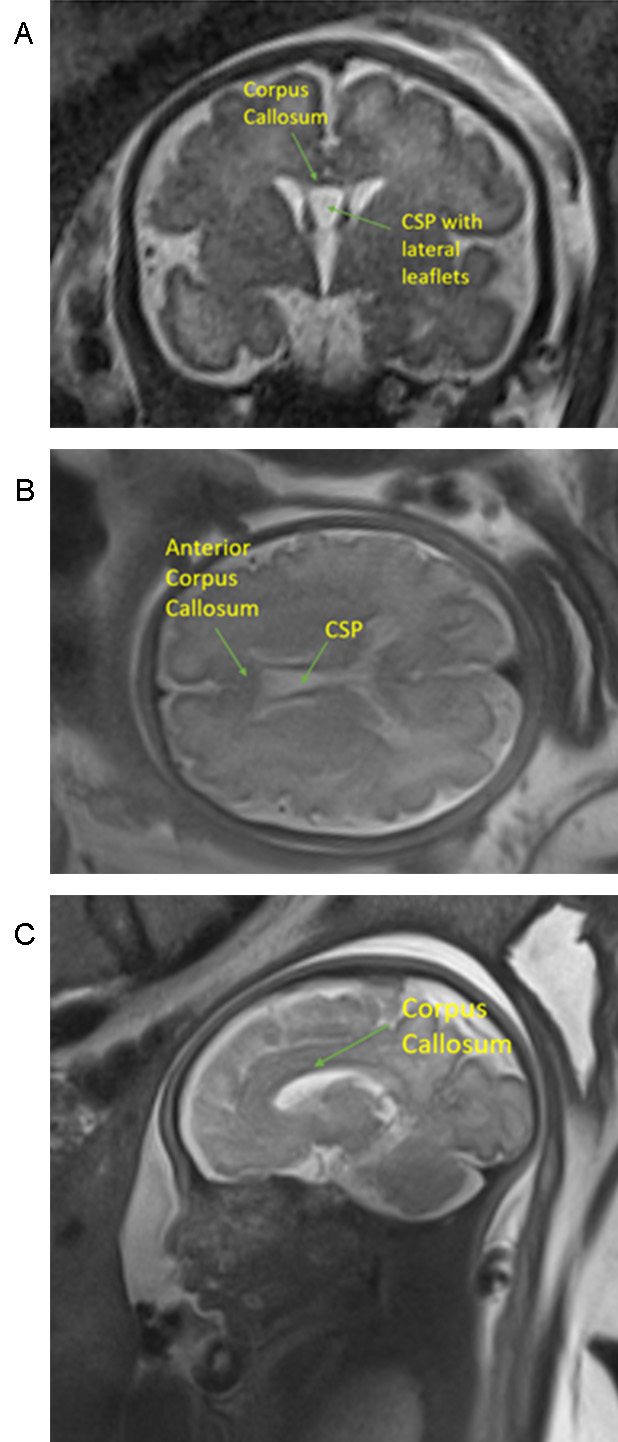
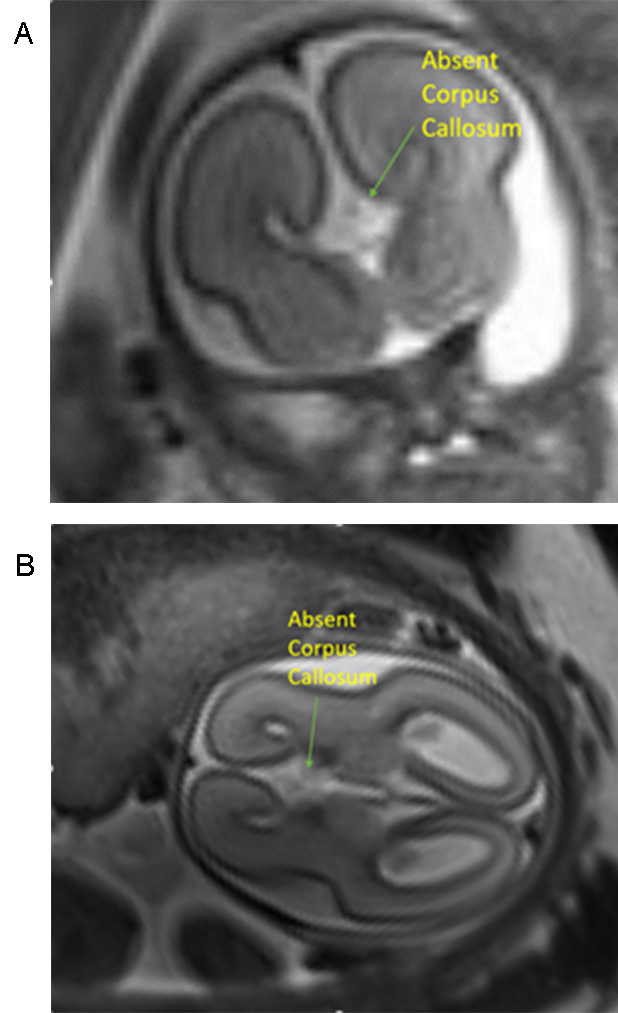
Figure 4. Abnormal MRI (consistent with Agenesis of the Corpus Callosum)
A. Coronal view with an absent corpus callosum linking the 2 halves of the brain and no separation noted between the anterior lateral ventricles
B. Axial view of the brain with no evidence of the anterior corpus callosum, no separation between the lateral ventricles and a dilated third ventricle
When ACC or PACC is suspected with ultrasound and/or MRI, providers assess if the finding is an isolated abnormality or one of many cerebral and/or extra-cerebral malformations (complex). Wide ranging abnormalities can be associated with a diagnosis of ACC or PACC making certainty of a truly isolated finding difficult within the prenatal time period. Common intracerebral abnormalities are concurrent brain abnormalities such as Dandy-Walker anomalies, vermian dysgenesis, septo-optic dysplasia, polymicrogyria, or other disorders of neuronal migration. In studies with suspected isolated ACC after an ultrasound or MRI, pathology studies of these fetuses have shown that the isolation diagnosis is only correct in approximately 10% of those studied. These data indicate that some diagnoses of additional anomalies cannot be made with prenatal imaging.
Extra-cerebral abnormalities are common in the setting of ACC and can impact a wide range of organ systems. Approximately 60% of cases of ACC have been found to have additional extra-cerebral anomalies, most commonly within the cardiac and genitourinary systems.
In most cases, the cause of ACC/PACC is unknown. It has been hypothesized that agenesis of the corpus callosum is associated with abnormal neural migration or incomplete maturation of the neurons that occurs when the brain initially forms. Others hypothesize that this disorder may be due to an infection or other environmental insults that occur as the brain develops. Additionally, there are many varied genetic causes that can be associated with this disorder and genetic testing is advised.
Currently, there are > 1,900 matches for ACC in the OMIM database, an online catalog of human gene and genetic disorders. This illustrates how complex the genetic and syndromic evaluation for this abnormality is. This condition has been found to have autosomal dominant, autosomal recessive, X-linked or sporadic genetic mutations and has also been found in patients without any genetic abnormalities. ACC has been reported as a feature in more than 200 different syndromes or metabolic diseases. Prenatal genetic testing allows families to gain information and better understand what other structural and functional findings can be expected based on the data obtained.
Individuals with ACC or PACC often have a genetic etiology which can be determined via genetic testing. Prenatally, the most sensitive and commercially available testing for fetuses with ACC is via amniocentesis with whole exome sequencing (WES). WES is a genetic testing method that analyzes the protein coding regions of the genome to identify pathogenic/likely pathogenic genetic abnormalities. In cases with isolated ACC, WES has detected a pathogenic/likely pathogenic genetic abnormality in 32% of cases. In more complex cases with ACC and extra-cranial abnormalities, WES has detected genetic abnormalities in 55% of cases. WES in ACC with additional intracranial anomalies has a 43% detection rate of genetic abnormalities. Despite the improved rates of finding genetic abnormalities with WES, there are still small gene mutations that cannot be detected with the genetic testing options available prenatally.
There has been a lot of variability in childhood outcomes associated with ACC over the years. Data regarding outcomes are generally limited to isolated ACC without defined genetic abnormalities and cannot necessarily represent those patients with ACC complicated by other physical or genetic abnormalities.
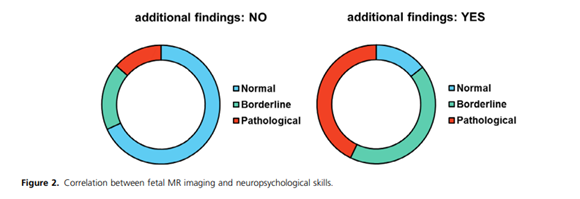
In a thorough prospective study, children with prenatally detected isolated ACC (confirmed by prenatal MRI) (median age 8.5 years) underwent age-appropriate physical exam, repeat MRI testing in childhood, genetic evaluation, and cognitive, motor and language evaluations to assess the impact of ACC. On entry into the study, 10% of these children were found to have additional physical findings on exam that were not previously detected. 21% of these children that were thought to have isolated ACC on their prenatal MRI were found to have additional brain abnormalities when they underwent a follow up MRI. 48% had genetic abnormalities when they underwent testing.
With regards to motor and cognitive testing, 62% of these children had normal results but this decreased to 44% when undergoing testing for language development. Almost half of all of the children were already enrolled in rehabilitation programs for speech and motor therapy (45% and 40% respectively) prior to involvement in the study.
Romaniello R et al:
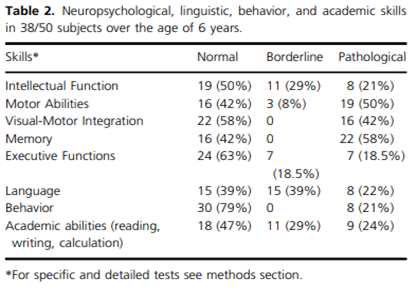
Romaniello R et al:
Studies evaluating adults with ACC are generally less robust than childhood data; often revolving around case studies or cross-sectional survey studies. These studies have potential ascertainment biased by evaluating individuals whose diagnosis were already made in childhood due to recognized cognitive deficits. Additionally, adult testing in these settings has often focused on IQ testing or other laboratory structured tests which can be within the normal range but not representative of how these individuals function in the world.
As a result of the underlying pathophysiology of an absent corpus callosum, deficiencies in interhemispheric transfer of sensory motor information are common. Due to the lack of the standard interhemispheric communication pathway, compensatory networks in other regions in the brain have been found to aid in baseline functioning. Neuropsychological research has been performed to assess executive function in adults with ACC and have found mild to moderate deficiencies in concept formation, complex problem solving, memory encoding, and psychosocial understanding with a wide range of deficit severity. Adaptive behaviors are also an area of deficiencies in individuals with ACC despite being high functioning on other laboratory tests. Study of adaptive behaviors displayed delays in social and practical skill in areas of meeting personal needs and interacting with others. Unfortunately, all of these studies in adults are limited and cannot be universally applied to the prenatal diagnosis of ACC.
There are no curative treatments to repair the absent corpus callosum for this disorder either pre- or postnatally. Available treatments for ACC revolve around the symptoms that are detected during childhood. For example, seizures can be treated with anti-epileptic medications and other findings such as intellectual or motor delays can be treated with special education and physical/occupational therapy. Other therapies that may be required include ventriculoperitoneal shunts for cases with hydrocephalus, speech and visual rehabilitation for speech/visual problems, and psychiatric therapies.
We know that in cases of prenatally detected ACC by ultrasound and MRI, approximately 31% of the pediatric evaluations detect other abnormalities (intra- and/or extra-cranial) utilizing childhood MRI and/or physical exam. Based on autopsy specimens of fetuses diagnosed with isolated ACC, the chance of additional abnormalities is higher as has been detected by pathologists. As such, there are significant limitations for detection of potential abnormalities during the prenatal time frame despite the best imaging available during pregnancy.
While approximately 64% of young children with isolated ACC had reportedly normal neurodevelopmental outcomes, the remaining 36% were found to have borderline, moderate or severe neurodevelopmental outcomes. Literature reviews of isolated testing in early childhood portend a favorable outcome in 2/3 of the cases, however, additional disabilities can arise in older school aged children. Unfortunately, there are no methods of predicting for certain outcomes in cases of prenatally diagnosed isolated ACC.
ACC in the setting of additional anomalies is also known to be associated with a higher chance for pathologic genetic abnormalities as well as more likely to have a higher likelihood of abnormal neuropsychological outcomes. Due to the limitations of detection of additional abnormalities during the prenatal time frame, exact expectation for neurologic outcomes cannot be stated with complete accuracy. Ultimately, in the prenatal period, families will have some degree of uncertainty regarding the long term outcomes in all settings of prenatally diagnosed ACC. Invasive genetic testing with use of higher level screening is advised if additional genetic information would be deemed useful by the family.
- Society for Maternal-Fetal Medicine, Rotmensch S, Monteagudo A. Agenesis of the corpus callosum. SMFM Consult Series, 2020. B17-B22
- Mustafa HJ, Barbera JP, Sambatur EV, Pagani G, Yaron Y, Baptiste CD, Wapner RJ, Brewer CJ, Khalil A. Diagnostic yield of exome sequencing in prenatal agenesis of corpus callosum: Systemic review and meta-analysis. Ultrasound Obstet Gynecol 2024; 63: 312-320. DOI: 10.1002/uog.27440
- Santo S, D’Antonio F, Homefray T, Rich P, Pilus G, Bhide A, Thilaganthan B, Papageorghiou AT. Counseling in fetal medicine: agenesis of the corpus callosum. Ultrasound Obstet Gynecol 2012; 40: 513-521. DOI: 10.1002/uog.12315
- Tsai P, Shinar S. Agenesis of the corpus callosum: What to tell expecting parents? Prenatal Diagnosis 2023; 43: 1527-1535. DOI: 10.1002/pd.6447
- Brown W, Paul L. The neuropsychological syndrome of agenesis of the corpus callosum. J Int Neuropsychol Soc. 2019 25(3): 324-330. DOI:10.1017/S135561771800111X.
- Romaniello R, Arrigoni F, DeSalvo P, Bonaglia MC, Panzeri E, Bassi MT, Parazzini C, Righini A, Borgatti R. Long-term follow up in a cohort of children with isolated corpus callosum agenesis at fetal MRI. Annals of clinical and translational neurology. 2021. 2028-2288. DOI: 10.1002/acn3.51484
- Miller J, Brown W, Mangum R, Nolty A, Paul L. Adaptive behavior in primary agenesis of the corpus callosum. Research in Developmental Disabilities. 2024, 154. DOI: 10.1016/j.ridd.2024.104862
DesPortes V, Rolland A, Velazquez-Dominguez J, Peyric E, Cordier MP, Gaucherand P, Massardier J, Massoud M, Curie A, Pellot AS, Rivier F, Lacalm A, Clement A, Ville D, Guibaud L. Outcome of isolated agenesis of the corpus callosum: A population-based prospective study. Eur J Paediatric Neurology. 2018, 22 (1) 82-92. - Raile V, Herz N, Promnitz G, Schneider J, Tietze A, Kaindl A. Clinical outcomes of children with corpus callosum agenesis. Pediatric Neurology. 2020. 112. 47-52. DOI: 10.10016/j.pediatrneurol.2020.07.013.
- Bernardes da Cunha S, Careneiro MC, Sa MM, Rodrigues A, Pina C. Neurodevelopmental outcomes following prenatal diagnosis of isolated corpus callosum agenesis: A systematic review. 2021, Fetal Diagn ther; 48: 88-95. DOI: 10.1159/000512534.