Congenital Epignathus
Congenital epignathus (from the Greek “epi” for “above” and “gnathos” for “jaw”) is an extremely rare form of teratoma (germ cell tumor) that arises from the oropharynx, the middle part of the throat, specifically from the hard palate. It is estimated that these tumors occur in approximately 1 in every 35,000 to 1 in every 200,000 livebirths (1). As a teratoma, all three primitive embryonal germ layers (endoderm, mesoderm and ectoderm) are present in these typically benign tumors that arise from Rathke’s pouch, which is an evagination or outpouching at the roof of the developing mouth in what will become the hard palate. Malignant or immature teratomas of the soft palate have also been reported and can include intracranial extension (2).
Congenital epignathus arise from the palate in the majority of cases and can be associated with cleft palate, tongue or nose anomalies (Figure 1) (3). Epignathus can grow to extremely large proportions but always has a narrow base arising from the palate with arterial blood supply solely from one or both palatine arteries. The mass may grow at such a fast rate that it can distend the mouth, causing mandibular dislocation of the temporomandibular joints bilaterally. The blood flow in these large epignathi may be sufficiently large to cause high output cardiac failure. Tumors sufficiently large to cause this volume of blood flow can literally “steal” from the baby causing growth arrest.
Epignathus tumors may be relatively easy to diagnose at birth but tumors have been diagnosed prenatally using real-time ultrasound for decades (4). Prenatal diagnosis can be critical as large epignathus can lead to airway obstruction and high mortality rates (5, 6).
In a review by Clement of cases reported in the literature between 1989 and 1999, 15 cases of epignathi were summarized (7). All but three were prenatally diagnosed and ranged in size from 2 to 17 cm. Cases were diagnosed in all trimesters but the majority were the third trimester. Of the cases that reported outcomes, 5 resulted in a perinatal death and 3 were elective terminations.
Prenatal detection of oropharyngeal tumors is primarily by ultrasound. Detection of epignathus may be aided by development of polyhydramnios, due to obstruction of swallowing prompting referral for ultrasound. In some cases, the epignathus may be functional secreting the tumor marker alpha-fetoprotein which may prompt referral for ultrasound. A case of congenital epignathus associated with a maternal serum alpha-fetoprotein (MSAFP) of 7.7 MoM at 15 weeks was reported leading to prenatal diagnosis by ultrasound at 17 weeks (7). In another case of elevated MSAFP of 5.1 MoM at 19 weeks ultrasound revealed an epignathus teratoma was also reported (8).
Congenital Epulis
Congenital epulis (from the Greek “epi” for “above” and “oulon” for “gum”) is a rare oral tumor arising from the alveolar ridge of the maxilla or mandible. These tumors, first reported in 1871 by Neumann, are granular cell tumors (9). The differential diagnosis includes hemangioma, fibroma, teratoma and granuloma. In an extensive review of the literature, Zuker reported on 195 lesions diagnosed starting from 1871 (9). The majority of cases were in females (10 to 1) and the tumors were twice as likely to be maxillary in origin, usually in the incisor or canine region. These lesions are typically solitary but can be multiple, smooth pedunculated tumors that range from several millimeters to many centimeters in size. Histogenesis of the tumors is uncertain but the predilection for females suggests a hormone sensitive tissue of the origin. Postnatal observation of epulis tumors often show progressive involution (shrinkage) consistent with hormonal influence with withdrawal of pregnancy related hormonal milieu. The histology of epulis is similar to other granular cell tumors (10).
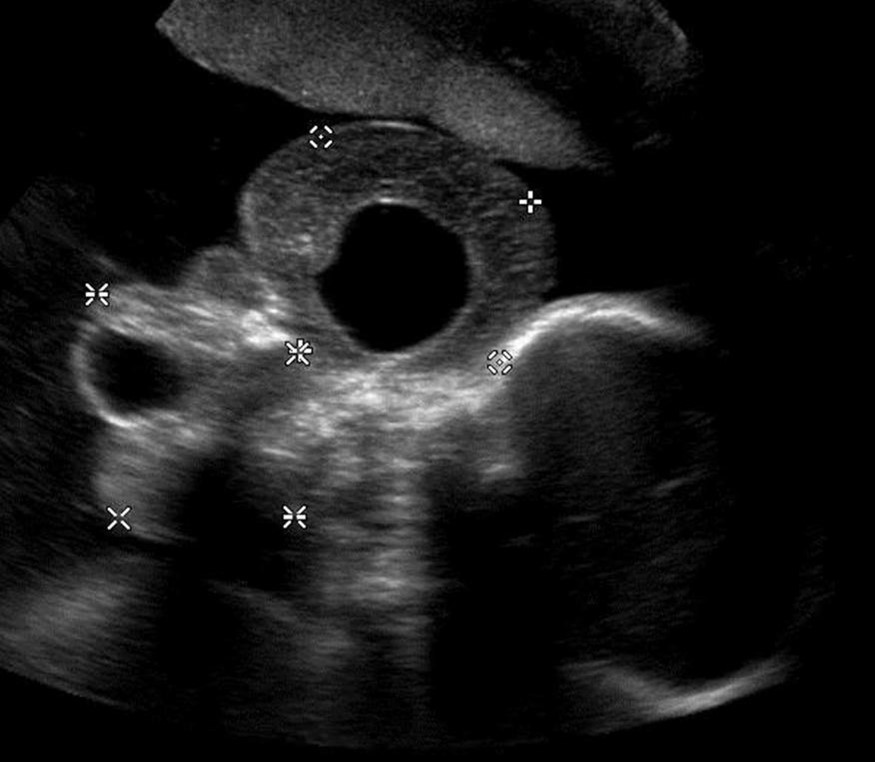
Ultrasound is the primary mode of detection of congenital oropharyngeal tumors such as epignathus and epulis. Epignathus can have a varied presentation by ultrasound. The tumors tend to be complex with cystic and solid components and color-flow Doppler can demonstrate blood supply from the palatine arteries (Figure 3.). Epignathus, being a teratoma, has a greater propensity to grow to significant dimensions. Due to their origin in the hard palate when they enlarge, they obstruct the fetal airway and may distend the mouth to the extent that the temporomandibular joints become dislocated. Both 2-D and 3-D ultrasound have been used to diagnose and characterize congenital epignathus (14, 15, 16). Shih reported using 3-D ultrasound reconstruction of the upper airway to virtually determine if intubation could be possible in a case of epignathus. In this case, MRI confirmed the diagnosis and probable airway compromise, and an EXIT procedure was planned due to the extent of the tumor.
Figure 1
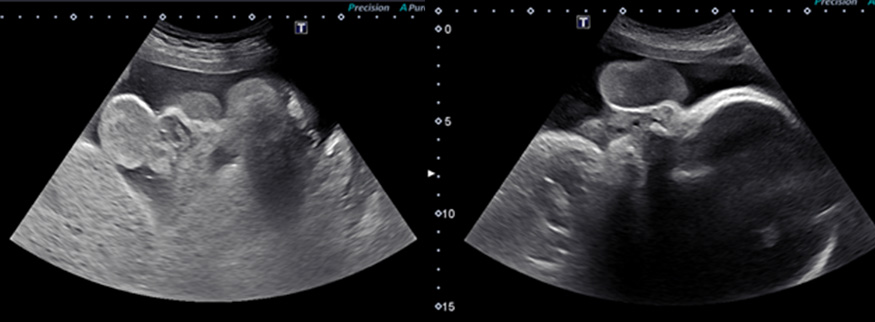
Congenital epulis typically arise in the second or third trimester. They appear as well-defined round masses near the naso-labial junction arising from the alveolar ridge of the mandible or maxilla but commonly from the maxilla (11, 12). The vast majority of congenital epulis are solitary although numerous cases of multiple lesions have been reported (Figure 2) (13). Unlike epignathus, epulis tends to be smaller, may be multiple and compromise of the airway is less common. Increased blood supply through a vascular pedicle is typical. No other fetal anomalies have been reported to be associated with congenital epulis but the differential diagnoses when prenatally detected includes other oral-facial masses such as hemangioma, sarcoma, and granular cell myoblastoma.
Figure 2
Accurate prenatal diagnosis and establishment of the extent of a congenital epignathus or epulis is important to plan for delivery room management. The use of 3-D ultrasound has been described in the evaluation of facial masses, but MRI may be more helpful in elucidating the origin of facial tumor (15). Due to the larger field of view with fetal MRI, a better appreciation of the dimensions of the epignathus and the narrow base on the hard palate can be obtained (Figure 3). If blood flow to the epignathus is sufficiently large, the flow voids caused by the palatine arteries can be visualized (Figure 3).
Figure 3
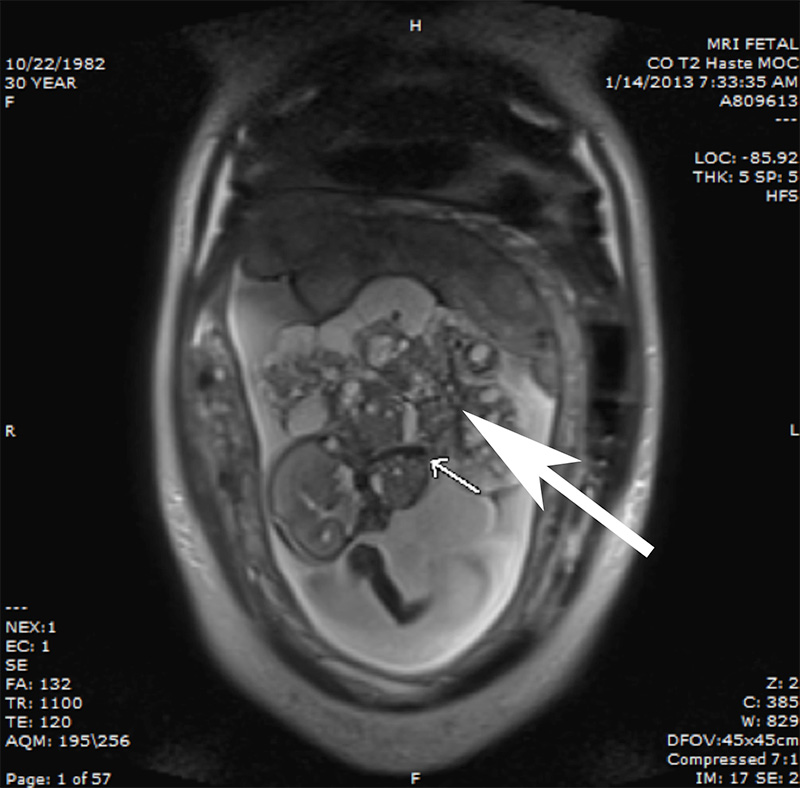
MRI has also aided in the diagnosis of congenital epulis (15). On MRI, epulis tends to be a discrete mass with smooth borders arsing from the ginginva (17). Roy and colleagues reported a case of congenital epulis that was diagnosed at 38 week’s gestation by prenatal ultrasound (18). Two small lesions were noted to be protruding from the fetal mouth. Fetal MRI using a HASTE sequence confirmed the diagnosis of epulis showing homogeneous tumors of low signal intensity on T1-weighted images arising from the mandible and maxilla. Congenital epulis tends to have isointensity with muscle on T1-weighted imaging and isogeneous to heterogeneous signal intensity on T2-weighted imaging (19). Additional reports indicate congenital epulis can display a similar signal to muscle on T1-weighted imaging or iso- to heterogeneous signal intensity on T2-weighted imaging.
A possible limitation of MRI is that it cannot provide functional information on possible airway obstruction after birth. In the absence of polyhydramnios, preservation of fluid in the oropharynx has been used on MRI to suggest that the airway has not been compromised (16). Bornstein and colleagues described sonographic functional assessment of congenital epulis including fetal breathing and swallowing, presence and severity of polyhydramnios or an absence of a stomach bubble, and bidirectional flow of fluid from the nares to assist in deciding airway compromise and delivery room management with the need for a possible EXIT procedure (19). We view ultrasound and fetal MRI as complimentary imaging modalities essential in determining the appropriate delivery management of epignathus and epulis.
Typically, epulis and epignathus are isolated tumors in the oropharynx and are not reported to be associated with congenital heart disease. However, due to reports of hydrops associated with epignathus, fetal echocardiography to assess cardiac function may be warranted. Especially in the setting of a large epignathus, echocardiographic assessment of combined ventricular output may provide an initial baseline and may be an indication for fetal intervention if this becomes markedly elevated. A diagnosis of high output heart failure may also assist in timing of delivery or discussions of palliative care, depending on gestational age.
Although data is limited, based on case reports and small series, the diagnosis of oropharyngeal tumors after previously normal anatomy ultrasound scans suggests epignathi form during late second and early third trimester (4, 19). In contrast, epulis has been diagnosed as early as 15 weeks’ gestation. While epignathus has broad range of sizes which may or may not compromise the fetal airway, epulis tends to be smaller and less likely to cause polyhydramnios or airway obstruction. Development of pregnancy complications such as polyhydramnios is common in cases of large epignathus. This suggests potential airway obstruction. Also, fetal hydrops from high output cardiac failure has been reported (21). Preterm birth has been reported in numerous cases of epignathus due to preterm premature rupture of membranes (PPROM), pre-term labor and abruption (22, 23). Polyhydramnios is likely a risk factor for such pregnancy complications. In cases in which epignathus grows to significant proportions, the mass effect on the mandible may cause the temporomandibular joints to dislocate. In this setting, the airway is invariably compromised. Similarly, large epignathus tumors can develop a vascular and metabolic “steal” causing growth arrest in the fetus.
Monitoring pregnancies for growth of oropharyngeal tumors is needed to plan the best mode and timing of delivery. Once a clear diagnosis of epulis or epignathus is made by ultrasound and MRI, ultrasound monitoring for growth of the tumor or potential spread of an epignathus is recommended. Additional monitoring is for the development of polyhydramnios or signs of fetal hydrops should be serially assessed by ultrasound. The frequency of follow up should be guided by the size of the mass. Fetal grow should also be monitored in cases in which the tumor is large for signs of fetal growth restriction. Color Doppler of the mass should be used to assess the vascularity of the tumor. In cases in which there is rapid increase in the size of the mass, development of polyhydramnios, or fetal growth restriction should prompt fetal echocardiographic assessment of combined ventricular output. Abnormalities in these parameters may inform decision-making regarding fetal intervention or delivery planning.
There are several options for fetal intervention in epignathus and epulis. Epulis rarely becomes so large as to cause polyhydramnios or high output failure during mid-gestation. More often, in epulis, the mass is modest in size and does not compromise the fetal airway. Epignathus, in contrast, can grow to enormous proportions sometimes the size of the entire fetus. Decision-making in the management of epignathus will depend on gestational age, presence or absence of polyhydramnios, high output state, signs of hydrops, growth restriction and evidence of fetal airway compromise. Patients less than 30 weeks’ gestation with these complications are at risk for intrauterine fetal demise, preterm premature rupture of membranes, preterm labor and delivery with attendant risks of prematurity.
Fetal surgery has been reported for epignathus. Kontopoulos reported a case of isolated epignathus with no evidence of spread (25). A feeding artery was identified by Doppler ultrasound and tumor resection was accomplished by fetoscopic transection of the stalk. Caution is advised for fetal treatment as there can be associated clefts and extension of the tumor not appreciated by fetal imaging. Especially when epignathus presents in association with cleft palate, one should consider the impact of treatment on the palatal blood supply upon which the palatal flap for cleft palate repair will depend. Other pregnancy management may include therapeutic amniocentesis for cases of severe polyhydramnios or premature delivery for cases of hydrops (21).
Ultrasound guided intravascular coagulation is a less invasive approach to treating giant epignathus complicated by hydrops, high output failure, or growth restriction from vascular steal. This approach has been used successfully in the management of bronchopulmonary sequestration and sacrococcygeal teratoma in selectively devascularizing the tumor (26). Epignathus is uniquely suited to this form of intervention as the mass derives its entire blood supply from the palatine arteries. These feeding vessels can be demonstrated within the mass by color Doppler in cases manifesting complications related to large volume of blood flow. An 18-gauge needle can be ultrasound guided to the palatine artery at the base of the tumor and a 600-micron Endostat advanced into the vessel and photocoagulated. The palatine arteries should be treated within the exophytic mass of the epignathus to avoid vessel rupture and hemorrhage as well as compromise of the blood supply of the palate. This can be repeated within the tumor to treat branches of the left and right palatine arteries until the exophytic portion of the epignathus is completely devascularized. The interruption of blood flow to the tumor will normalize the combined ventricular output and eliminate vascular steal. Necrosis of the mass will result in progressive reduction in the size of the mass and improvement in polyhydramnios. As the gestation progresses, ongoing assessment for the need for EXIT strategy for delivery is important as the size of the residual mass may still compromise the airway.
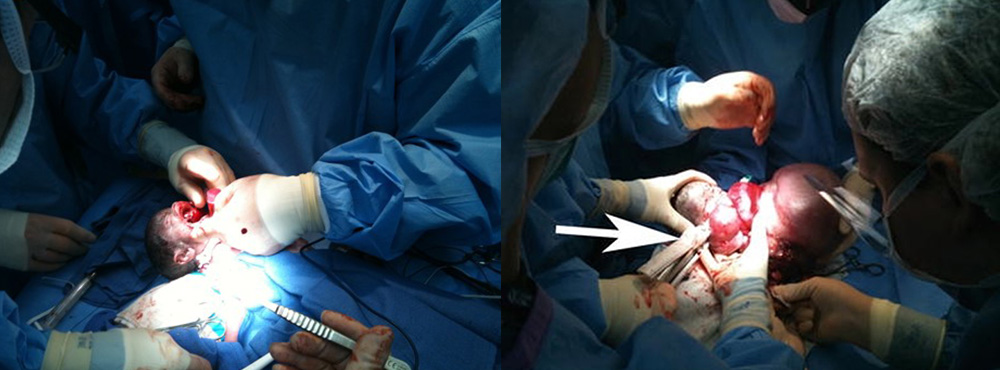
After 30 weeks’ gestation, if hydrops, severe polyhydramnios, vascular steal, or high output state with combined ventricular output greater than 600 ml/kg/min develops, serious consideration should be given to EXIT-to-Resection. The narrow base of origin on the hard palate in epignathus makes even a very large exophytic tumor relatively easy to deal with by stapling across the base of the tumor with a thick tissue GIA stapler (Figure 4). Depending upon the maternal-fetal stability, a complete resection of the residual tumor from the palate can be performed during the EXIT procedure or can be deferred until after the baby is stabilized following delivery.
Figure 4
Delivery Management
For prenatally diagnosed oropharyngeal tumors, delivery at a hospital with pediatric subspecialists is warranted. An experienced fetal treatment center with pediatric surgery, ENT and Obstetric and Pediatric Anesthesia may be critical in establishing an airway at delivery. In cases where airway obstruction is likely, delivery at a center capable of an EXIT procedure is most likely to result in establishing an airway and initial treatment of epulis and epignathus, when warranted. In cases in which airway compromise is uncertain but not thought to require an EXIT procedure, delivery with an airway team standing by is advisable.
A cesarean is the prudent approach for delivery of prenatally diagnosed congenital oropharyngeal tumors when there is concern for airway obstruction. The most important reason for cesarean is the ability to maintain fetal-maternal circulation while evaluating the degree of tumor and establishing an airway, whether by intubation (oral or nasal) or tracheotomy, if needed. For large tumors, dystocia or tumor rupture may be a concern, even at cesarean, requiring careful planning for the approach to the skin and uterine incisions. The uterine incision may need to be vertical if the lower uterine segment is small or if extension is needed to manipulate the fetus for intervention. Alternatively, depending on placental location, a lower uterine segment incision can be made with a “hockey stick” extension on one side may provide sufficient exposure to allow delivery of the fetal head and oropharyngeal mass without undue trauma to the tumor.
For cases of epignathus with extensive disease, particularly with extension to the CNS, palliative care may be an option. If this has been agreed upon prior to delivery and dystocia of the tumor is not a concern, a vaginal delivery may save morbidity for the mother.
Timing of delivery must be individualized in case of oropharyngeal tumors. Epulis is usually smaller and more localized than epignathus; a planned near-term delivery can be considered. Epignathi tend to be larger and may have local or CNS extension. For complex cases, the timing of delivery may be dictated by prenatal complications leading to a preterm birth. If airway complications are expected based on prenatal imaging and secondary factors such as polyhydramnios, a planned delivery may be warranted. If an EXIT delivery is required, a planned, early term delivery can allow for assembly of the multidisciplinary team needed for such an approach. In cases requiring EXIT strategy due to airway compromise, a “telephone tree” should be put in place to quickly mobilize the EXIT team members should the patient go into labor prior to the planned EXIT date.
Delivery Planning
The intrapartum management of epignathus and epulis depends on the size of the tumor and the concern for airway obstruction. Catalano reported the performance of a tracheostomy at the time of cesarean prior to interruption of fetal-maternal circulation for a large epignathus tumor at high risk for airway obstruction (27). Ruano reported a case of epignathus in which a 3D ultrasound showed a clear nasopharyngeal passage and delivery was performed without an EXIT (16). Despite reports of EXIT and non-EXIT approaches to epignathus, the size, location and secondary markers of the potential for airway obstruction after birth must dictate the treatment at delivery. This is highlighted by the high rate of mortality for epignathi not diagnosed prenatally.
In a 6-year review of oropharyngeal tumors at CHOP, there were four cases in which an EXIT procedure was performed, two were epignathus and two epulis (28). All were diagnosed in the third trimester between 29 and 34 weeks. The two cases of epignathus developed polyhydramnios while the two with epulis did not. The epulis tumors were 2 and 4 cm and were resected at the time of EXIT after intubation was performed. The epignathus cases were 8 cm and 14 cm and tumor resections were delayed.
In general, EXIT procedures should be reserved for cases at high risk for airway compromise. However, in cases in which intubation of the baby would be difficult, it is best to have an airway team standing by at the delivery. This would include either a Pediatric Otolaryngologist or Pediatric Surgeon with ability to intubate over a rigid rod lens or flexible bronchoscope. If there is reason to believe that standard intubation would be difficult, the airway team should secure the airway, even though the baby may show no signs of respiratory distress, until the mass can be resected. Although rarely necessary, the airway team should also be prepared perform a tracheostomy should be attempts at orotracheal or nasotracheal intubation fail.
While rare, congenital epulis are benign tumors readily diagnosed with prenatal ultrasound and can be confirmed by MRI. As these are easily resected after birth, there is limited role for palliative care. Congenital epignathus can also be readily detected with prenatal ultrasound. MRI is important in establishing the extent of the tumor. As a teratoma, there is a small but finite risk for immature or malignant transformation with the potential for local spread. Intracranial spread with CNS involvement has been reported in epignathus. In such cases, there may be role for extensive patient counseling on management options including the role of pregnancy termination or postnatal palliative care options (2, 29).
Postnatal Management
At the time of delivery of a baby with epignathus or epulis, a detailed physical examination of the baby should be performed with the first priority being the patency of the airway. If there is any question as to the difficulty in obtaining an airway, it is best to intubate prophylactically to secure the airway. This can be done nasotracheally over a flexible bronchoscope or orotracheally over a rod lens if unable to place a laryngoscope blade into the oropharynx. Alternatively, in the case of epignathus, which may be large, the tumor can be expeditiously dealt with by firing a thick tissue GIA stapler (Covidien, Dublin, Ireland) across the base of the tumor. The residual tumor will remain on the hard palate which will require subsequent resection, but this approach clears the oropharynx for intubation, if required.
MRI with contrast provides excellent delineation of the extent of the tumor, involvement of the alveolar ridge and the tooth buds. If present, cleft lip and palate can also be assessed as well. In epulis, the mass often displaces the tooth buds and has a smooth well defined margin that allows it to be shelled out at the time of surgery. In epignathus, the tumor usually extends to the boney hard palate.
While there is no medical management for epignathus or epulis, there may be a role for expectant management in epulis. These tumors can be relatively small and, if they do not interfere with bottle feeding, can be managed expectantly. There are reports suggesting that epulis is sensitive to maternal hormones during pregnancy, once delivered, regress on their own. Expectant management has the advantage of not putting the tooth buds in the alveolar ridge at risk during resection. However, expectant management should be considered only in cases in which bottle or breast feeding is possible despite the epulis.
A major consideration in the surgical management of and epignathus or epulis is the timing of surgery, and as may be the case epulis, whether surgery is needed at all. We have already discussed the role of EXIT procedures in the management of oropharyngeal tumors. In cases in which a stable airway has been obtained, there is no urgency regarding resection. However, if obtaining the airway is difficult due to the size of the mass obstructing the oropharynx, it is prudent to proceed with resection expeditiously. In the case of epignathus, even if the mass is extremely large, the origin of the tumor will have a narrow base on the hard palate. Access to the base of the tumor can be facilitated by stapling off the epignathus just beyond the alveolar ridge. This allows the extent of the involvement to be fully assessed and complete excision can be completed then or electively if the baby is unstable for other reasons. Epignathus is usually a benign teratoma which can recur locally if incompletely excised. Excision of the mass down to the boney palate will prevent recurrence and heals rapidly in the newborn. One caveat to this approach is in the setting of an associated cleft palate in which the palatal blood supply to future flaps used for cleft palate repair may be compromised. In this instance, it may be advisable to perform the resection with the assistance of the Pediatric Plastic and Reconstructive Surgeon who will eventually perform the cleft palate repair.
In the case of epulis, thought should be given to whether or not the mass or masses should be excised or managed expectantly. If they are small enough not to interfere with oral feeding, these lesions may regress on their own. In cases of large lesions, resection will be needed to avoid airway compromise and allow oral feeding. Epulis tends to have a well circumscribed border or have a pedunculated base arising from the alveolar ridge of either the mandible or maxilla. It may displace the tooth buds but does not disrupt them, and dissection along the well-defined capsule should avoid injury to the tooth buds. In cases of pedunculated lesions, excision at the alveolar ridge protects the tooth buds.
Local recurrence is possible with both epignathus and epulis so follow up for a year after resection is advisable. In the case of epignathus, because it is a teratoma, there is a low risk of malignant transformation if left in situ in an otherwise benign tumor. In contrast, epulis is a granular cell tumor, and even if incompletely resected, the residual tumor may regress on its own presumably secondary to the absence of maternal hormones sustaining it in utero.
Outcome Data & References
Due to the rarity of oropharyngeal tumors such as epignathus and epulis, little information on outcomes is available besides case reports and small series. In a series of 15 epignathi reported by Clement, three resulted in terminations of pregnancy, five in perinatal death with five survivors. The size of the lesions did not necessarily predict outcome; but factors to consider were size, spread and degree of airway obstruction. Recurrence after surgical resection was rare (7).
Congenital epulis are typically managed with surgical resection postnatally. Zuker reported a review of 167 cases of congenital epulis noting no recurrences after postnatal treatment; some cases showed full involution even after incomplete resection (9).
Although not typical, cases of chromosomal abnormalities associated with epignathi have been reported including ring X chromosomes, monosomy X, and other rare, sporadic chromosomal abnormalities (30-34). Amniocentesis should be considered for prenatal diagnosis of fetal chromosomal abnormalities. Familial recurrence has not been reported in the literature.
- Becker S, Schön R, Gutwald R, et al. A congenital teratoma with a cleft palate: report of a case. Br J Oral Maxillofac Surg. 2007;45(4):326-327.
- Kirishima M, Yamada S, Shinya M, et al. An autopsy case of epignathus (immature teratoma of the soft palate) with intracranial extension but without brain invasion: case report and literature review. Diagn Pathol. 2018;13(1):99.
- Kumar B, Sharma SB. Neonatal oral tumors: congenital epulis and epignathus. J Pediatr Surg. 2008;43(9):e9-e11.
- Levine AB, Alvarez M, Wedgwood J, Berkowitz RL, Holzman I. Contemporary management of a potentially lethal fetal anomaly: a success sful perinatal approach to epignathus. Obstet Gynecol. 1990;76(5 Pt 2):962-966.
- ElSherbiny Hamed M, El-Din MHN, Abdelazim IA, Shikanova S, Karimova B, Kanshaiym S. Prenatal Diagnosis and Immediate Successful Management of Isolated Fetal Epignathus. J Med Ultrasound. 2019;27(4):198-201.
- Jadhav SS, Korday CS, Malik S, Shah VK, Lad SK. Epignathus Leading to Fatal Airway Obstruction in a Neonate. J Clin Diagn Res. 2017;11(1):SD04-SD05.
- Clement K, Chamberlain P, Boyd P, Molyneux A. Prenatal diagnosis of an epignathus: a case report and review of the literature. Ultrasound Obstet Gynecol. 2001;18(2):178-181.
- Smart PJ, Schwarz C, Kelsey A. Ultrasonographic and biochemical abnormalities associated with the prenatal diagnosis of epignathus. Prenat Diagn. 1990;10(5):327-332.
- Zuker RM, Buenechea R. Congenital epulis: review of the literature and case report. J Oral Maxillofac Surg. 1993;51(9):1040-1043.
- Kumar P, Kim HH, Zahtz GD, Valderrama E, Steele AM. Obstructive congenital epulis: prenatal diagnosis and perinatal management. Laryngoscope. 2002;112(11):1935-1939.
- Jiang L, Hu B, Guo Q. Prenatal sonographic diagnosis of congenital epulis. J Clin Ultrasound. 2011;39(4):217-220.
- Frisova V, Prosova B, Mahdian N, Kyncl M, Vlk R, Rocek M. Prenatal diagnosis of congenital epulis by 2D/3D ultrasound and magnetic resonance. Fetal Diagn Ther. 2013;33(4):272-276.
- Liang Y, Yang YS, Zhang Y. Multiple congenital granular cell epulis in a female newborn: a case report. J Med Case Rep. 2014;8:413.
- Allen LM. Prenatal 3-dimensional imaging techniques in the sonographic evaluation of an oral mass: comparison with postnatal imaging modalities. J Ultrasound Med. 2011;30(4):561-568.
- Shih JC, Hsu WC, Chou HC, et al. Prenatal three-dimensional ultrasound and magnetic resonance imaging evaluation of a fetal oral tumor in preparation for the ex-utero intrapartum treatment (EXIT) procedure. Ultrasound Obstet Gynecol. 2005;25(1):76-79.
- Ruano R, Benachi A, Aubry MC, Parat S, Dommergues M, Manach Y. The impact of 3-dimensional ultrasonography on perinatal management of a large epignathus teratoma without ex utero intrapartum treatment. J Pediatr Surg. 2005;40(11):e31-e34.
- Roy S, Sinsky A, Williams B, Desilets V, Patenaude YG. Congenital epulis: prenatal imaging with MRI and ultrasound. Pediatr Radiol. 2003;33(11):800-803.
- Kim YD, Kim HJ, Lee NK, Ha WH, Lee CH, Park SF: Congenital epulis: prenatal ultrasonographic and postnatal MRI features with pathologic correlation. Oral Surg Oral Med Pathol Oral Radiol Endod 2000; 106:743-748
- Johnson KM, Shainker Sa, Estroff JA, Rolston SJ: Prenatal diagnosis of congenital epulis: Implications for delivery. JUM 2016; 36(2): 449-451
- Bornstein E, Boozarjomehri F, Monteagudo A, Santos R, Milla SS, Timor-Tritsch IE. Diagnostic and prognostic aspects in the sonographic evaluation of a fetus with an oral mass. J Ultrasound Med. 2009;28(5):689-693.
- Ekici E, Soysal M, Kara S, Dogan M, Gokmen O. Prenatal diagnosis of epignathus causing acute polyhydramnios. Acta Obstet Gynecol Scand. 1996;75(5):498-501.
- Kaplan C, Perlmutter S, Molinoff S. Epignathus with placental hydrops. Arch Pathol Lab Med. 1980;104(7):374-375.
- Chung JH, Farinelli CK, Porto M, Major CA. Fetal epignathus: the case of an early EXIT (ex utero intrapartum treatment). Obstet Gynecol. 2012;119(2 Pt 2):466-470.
- Santana EF, Helfer TM, Piassi Passos J, Araujo Júnior E. Prenatal diagnosis of a giant epignathus teratoma in the third trimester of pregnancy using three-dimensional ultrasound and magnetic resonance imaging. Case report. Med Ultrason. 2014;16(2):168-171.
- Kontopoulos EV, Gualtieri M, Quintero RA. Successful in utero treatment of an oral teratoma via operative fetoscopy: case report and review of the literature. Am J Obstet Gynecol. 2012;207(1):e12-e15
- Rodrigo Ruano 1, Marcos Marques da Silva, Eugenia Maria Assunção Salustiano, Mark David Kilby, Uenis Tannuri, Marcelo Zugaib. Percutaneous laser ablation under ultrasound guidance for fetal hyperechogenic microcystic lung lesions with hydrops: a single center cohort and a literature review Prenat Diagn 2012; 32(12):1127-32.
- Catalano PJ, Urken ML, Alvarez M, et al. New approach to the management of airway obstruction in "high risk" neonates. Arch Otolaryngol Head Neck Surg. 1992;118(3):306-309.
- Laje P, Howell LJ, Johnson MP, Hedrick HL, Flake AW, Adzick NS. Perinatal management of congenital oropharyngeal tumors: the ex utero intrapartum treatment (EXIT) approach. J Pediatr Surg. 2013;48(10):2005-2010.
- Smith NM, Chambers SE, Billson VR, Laing I, West CP, Bell JE. Oral teratoma (epignathus) with intracranial extension: a report of two cases. Prenat Diagn. 1993;13(10):945-952.
- Witters I, Moerman P, Louwagie D, Van Assche FA, Migeon BR, Fryns JP. Second trimester prenatal diagnosis of epignathus teratoma in ring X chromosome mosaicism with inactive ring X chromosome. Ann Genet. 2001;44(4):179-182.
- Arora V, Bijarnia Mahay S, Rao S, et al. The fatal fetal tumor: a geneticist's perspective. J Matern Fetal Neonatal Med. 2019;1-3.
- Beverstock GC, Mollevanger P, Baaij M, et al. Nasopharyngeal teratoma and mosaic tetrasomy 1q detected at amniocentesis. A case report and review of the literature. Cancer Genet Cytogenet. 1999;115(1):11-18.
- Schwartz S, Raffel LJ, Sun CC, Waters E. An unusual mosaic karyotype detected through prenatal diagnosis with duplication of 1q and 19p and associated teratoma development. Teratology. 1992;46(4):399-404.
- Staboulidou I, Miller K, Göhring G, Hillemanns P, Wüstemann M. Prenatal diagnosis of an epignathus associated with a 49,XXXXY karyotype--a case report. Fetal Diagn Ther. 2008;24(3):313-317.