When it comes to teaching children about their own cancer diagnosis, a step-by-step approach can be helpful. Talk to your child about each step of the treatment process as it’s happening. Connecticut Children’s Child Life team explains…
When your child is being diagnosed with cancer
Often, families may not have a confirmation that their child has cancer until after a biopsy. It can be helpful to explain to a child that they have a tumor (such as in brain cancer) or that the child’s blood is sick (such as in blood cancers like leukemia or lymphoma).
For solid tumors, you might say something like:
“When your doctors took the picture of your body, they saw a lump that’s not supposed to be there. This lump is called a ‘tumor’. A tumor is a lump inside your body that has no job. It just takes up space and makes it harder for your body parts to do their jobs. The doctors are still doing some investigating to figure out what this lump is made out of. That’s why you’re having the tests done.”
For leukemia or lymphoma, you might say something like:
“When your doctors looked at your blood under the microscope, they found out that your blood is sick.”
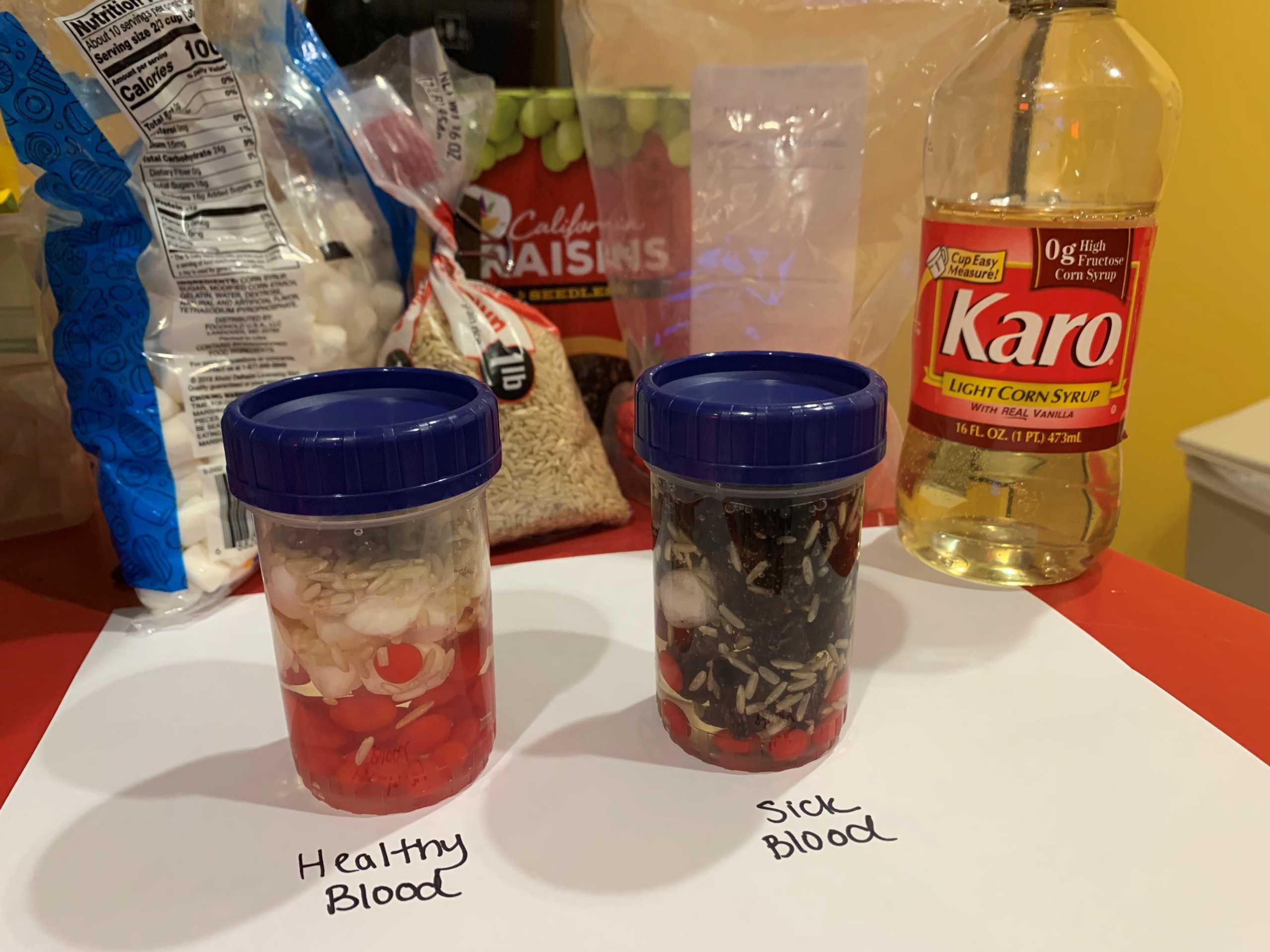
Connecticut Children’s Child Life will explain the roles of the different blood cells. Using an activity called “blood soup,” a child life specialist can help younger children visualize and differentiate healthy blood versus sick blood.
Once the cancer diagnosis has been confirmed
One example of how you may discuss your children’s cancer diagnosis is shown below:
“We came to the emergency room together because you were (insert symptoms). That’s when we knew something wasn’t right. Doctors are like detectives solving a mystery. They gather different clues through things like bloodwork or taking pictures of your body (i.e. MRI, ultrasound, x-ray). When your doctors put all these clues together, they figured out that you have something called ‘cancer’”.
Then, use simple, accessible terms to explain cancer. Another example is as follows:
“Our bodies are made up of little parts called cells. Each cell, or little part, has a job to do to keep us healthy. Some of the cells in your (blood, bones, etc.) grew too fast and didn’t learn to do their job. When this happens it’s called “cancer.” The cancer parts grow too fast and take up important space the healthy parts need to do their jobs. Your doctors have a plan to get rid of these parts so your body can feel better.”
Here are some important tips to remember:
- Explain that they didn’t do anything wrong that caused them to get cancer. Avoid using terms like “bad parts” or “mean parts” to explain “cancer.” Younger children often interpret this to mean they themselves are bad or mean.
- Inform your child that they did not catch cancer from someone and that no one else can catch cancer from them.
- Remind your child that painful things like shots are being done to help their body and are not a punishment. Our Child Life team is available to help your child build coping plans to increase comfort and decrease distress during procedures.
- Be aware of the dangers of Googling symptoms or diagnoses with older children and teens. Provide them with reliable resources and reassure them that childhood cancers are different from adult cancers, and each cancer is different.
- Reassure your child that the feelings they may be having are normal and acceptable. It’s ok to express the feelings you’re having, too – this will help your child feel comfortable approaching you. This is also a way for the child to express what is important to them in the moment. Children, for example, may be less worried about the future and more focused on missing their friend’s birthday party tomorrow. Open discussions can allow you to identify your child’s needs in the moment.
>Related: Why It’s Important to Talk Openly With Kids About Cancer
Talking to your child about cancer treatment
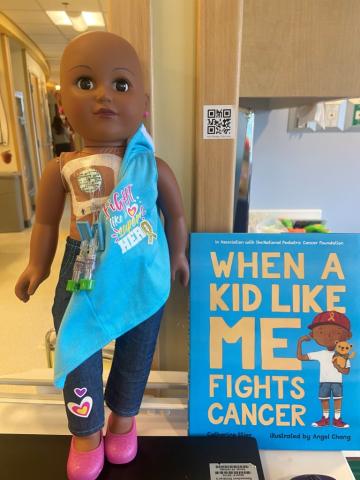
Some children may need surgery, some may need chemotherapy or radiation, and some may need all of these treatments. Many children may need a central venous line (a type of catheter) placed before beginning treatment. At Connecticut Children’s, our Child Life team will show what these look like on a doll or in a book.
You might tell your child the central venous line is like a medicine button (i.e., port) or set of helper tubes (i.e., Broviac catheter) that helps their body get strong medicine in a more comfortable way.
Children might also need to take medication by mouth. If your child does not know how to swallow pills, beginning this practice early can be helpful so that they are not trying to learn this skill while in a stressed state or up against a limited timeframe.
Addressing side effects of chemotherapy with children
Younger children:
When explaining potential side effects of chemotherapy to younger children, you might say something like, “Chemotherapy is a special kind of medicine that finds cancer cells in the body and gets rid of them. While it’s doing its job of getting rid of the cancer cells, chemotherapy can also make your tummy hurt and your hair fall out. This is not forever. Your hair grows back when you’re all done with treatment.”
Older children:
You may explain that chemotherapy targets “fast-growing cells” in the body. While chemotherapy targets faster growing cancer cells it may also affect faster growing healthy cells like hair cells and or cells lining your digestive system. This causes the common side effects of hair loss, nausea, or vomiting.
It can be helpful to identify other patients in the oncology clinic to demonstrate that everyone’s hair looks different (some may have short or long hair, and some may have no hair) because they may be at different points in their treatment.
Encourage self-expression when it comes to cancer-related hair loss:
You may offer choices for hair loss. Does the child want to try a new shorter hairstyle or dye their hair a crazy color? Does the child want to shave their head before their hair begins to fall out? Does the child want to “dress” their head after their hair falls out – would they like to wear a hat, scarf, or wig? It is important to give the child an opportunity to make decisions when so many other things are happening to their body that may be out of their control.
>Related: Expert-Approved Books to Get Through Tough Stuff

When faced with a cancer diagnosis, keep things as normal and routine as possible.
Maintain your parental role in your child’s life by continuing to set limits and upholding normal family responsibilities.
If your child or family is going through something difficult, it’s tempting to throw rules out the window. While this may feel good in the moment, in the long run it may negatively impact the way your child copes with challenges and develops important life skills. Setting limits helps children feel safer and in control. Children crave your guidance and support.
If you feel a reward system is the best motivator for your child and family, try to make the rewards family-centered – have your child choose the restaurant your family goes to or have them choose the movie for family movie night. This gives them what they really need – uninterrupted time to engage with the ones they love.
Always remember: regardless of which loved one in the family has cancer, talking openly about cancer with kids is important for many reasons.
>Related: Little Warrior: Jazz’s Story
